Royals Respond

Throughout the fall, The University of Scranton sports information office will be profiling former Royal student-athletes who are on the front lines in the battle against the spread of COVID-19. Read this story and others, here. Their fourth profile features Theresa (Kozlusky) Haley, a 1986 graduate former volleyball letterwinner.
During any student's undergraduate and postgraduate studies, they learn of situations that may come about in their prospective careers that will test their knowledge.
For Theresa Haley, it seems she’s prepared for over 30 years for the moment in time we are experiencing in 2020.
A former volleyball student-athlete and 1986 graduate with a degree in Medical Technology from The University of Scranton, Haley went on to earn a Certification in Infection Prevention and Control (CIC).
With this in tow, she eventually worked her way up to a position as an Iinfection preventionist at the Lebanon VA Medical Center where she serves as an expert on practical methods of preventing and controlling the spread of infectious disease. The hospital, as every VA does in the country, serves military veterans and is a part of the largest integrated health care system in the country, consisting of 170 medical centers.
As you can imagine, Haley’s life since March has been busy.
Right from the start of the pandemic, Haley and her team at the Lebanon VA went to work outfitting the hospital to prepare for the worst - a COVID outbreak in the community.
One of Haley’s main responsibilities from the start was repurposing a former intensive care unit into a “respiratory isolation unit" to treat potential coronavirus patients. The unit was equipped with an anteroom where staff members clean their hands and don protective equipment, including a mask that has an air filtration system. The unit is set up for negative pressure, which means the air goes through a filter before being released out of the environment.
Read on, here.
Theresa Haley ‘86 Prepares and Protects VA Hospital
VA infection preventionist and former volleyball student-athlete keeps patients, staff safe.
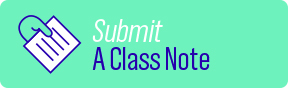
Nurses Andrew Graham '08 and Valerie Lucas '14 were part of the "heroic team" who treated their colleague at Memorial Sloan Kettering Cancer Center.
"I sat on the edge of the bed, held his hand, rubbed his heart, and we even at one point connected forehead to forehead. I don't think I've ever seen fear in a grown man's eyes like that in my entire life," said Graham in the piece reported by Hoda Kotb.
Watch the "Today Show" segment here.
Alumni Nurses Featured on 'Today Show'
Nurses Andrew Graham '08 and Valerie Lucas '14 were part of the "heroic team" who treated their colleague at Memorial Sloan Kettering Cancer Center.

Throughout the fall, The University of Scranton sports information office will be profiling former Royal student-athletes who are on the front lines in the battle against the spread of COVID-19. Read more, here.
The 2007 season for the then Meaghan Curtin was one for the record books on the defensive end for The University of Scranton volleyball team.
At the conclusion of the year, Curtin shattered the program record for digs, finishing the campaign with 811 to help Scranton win 25 games and advance to the very first Landmark Conference championship match. She also went on to earn All-Landmark Conference second-team honors, as well.
Now, in her professional life as the assistant nurse manager at Long Island Jewish Medical Center, the now Meghan Ledetsch is playing defense against a much stronger opponent -- COVID-19. Before taking her current position in July, Ledetsch served as a nurse in the Cardiac ICU at North Shore University Hospital in Manhasset, New York for five years, as challenging of a position as there is in the entire hospital.
“As one of the biggest Heart Center's on Long Island, I took care of the sickest of the sick cardiac patients,” Ledetsch said. “This includes but is not limited to carcinogenic shock, septic shock, end-stage heart failure, heart attacks, LVADS, heart transplants, arrhythmia's, pulmonary diseases, end-stage renal disease, etc. Sometimes these patients were so sick they needed to have two nurses instead of the 1-nurse to 2-patient ratio we typically have.”
But, even working in a high-pressure unit such as the Cardiac ICU could not prepare Ledetsch for what was to come this past spring. Once the pandemic reared its vicious head into the New York metro area in March, Ledetsch’s Cardiac ICU unit became a full-blown COVID ICU.
“Over the past few months, words cannot describe what my hospital has seen or gone through,” she said. “Myself and my colleagues were exposed to a whole different type of nursing.”
Ledetsch Adjusts on the Fly, Helps Long Island Block Back COVID-19
A former volleyball standout battles pandemic amid unprecedented circumstances outside New York City.

Throughout the Fall, The University of Scranton sports information office will be profiling former Royal student-athletes who are on the front lines in the battle against the spread of COVID-19. Their first profile features Kelly Johnson-Loughlin, a former volleyball student-athlete (2010-2013). Check their site for these profiles and athletics news.
In her playing days at Scranton, Kelly Loughlin (maiden name Johnson) was known for her blocking abilities at the net as a four-year letter winner for the volleyball team, finishing her career in the top ten all-time in two major statistical categories in program history - solo blocks (121, 6th all-time), and total blocks (265, 9th all-time).
Since March, Loughlin has been trying to block something else -- the spread of COVID-19 in her community.
A 2014 nursing graduate from The University of Scranton, Loughlin serves as an Emergency Room Nurse at The Queen's Medical Center in Honolulu, Hawaii, where she resides with her husband Dom and two dogs, Fetty and Kona.
At her job, Loughlin has been putting in 12-hour shifts to meet the demand COVID-19 has had in her hospital.
A native of Pearl River, NY, Loughlin has also experienced what many of us around the country have had to deal with - the reality of not being able to see friends and family that live far away.
“Living this far from home has been a challenge and now because of the pandemic we haven’t seen our family in over a year due to travel restrictions,” she said. “Hawaii has basically been on lockdown and making it very difficult to leave the island/return to the island. We had several trips home planned from February through September, all of them being cancelled.”
See more photos here.
Kelly Loughlin '14 Blocks COVID-19 Spread in Honolulu
A former Scranton volleyball standout fights the pandemic in Hawaii.
Karolyn Teufel, M.D. '98 co-authored a study alongside other George Washington University researchers that found five biomarkers were associated with higher odds of clinical deterioration and death in COVID-19 patients.
In a study of 299 COVID-19 patients who were admitted to GW Hospital between March 12 and May 9, 2020, they found that elevated levels of the biomarkers IL-6, D-dimer, CRP, LDH and ferritin meant an increased risk for ICU admission, invasive ventilatory support and death. This is an important finding, because it may help physicians in the U.S. better predict outcomes of COVID-19 patients.
“The association between biomarkers and clinical outcomes in novel coronavirus pneumonia in a US cohort” was published in Future Medicine and is available here.
Chemistry Alumna Co-authors Study on COVID-19
Karolyn Teufel, M.D. '98 coauthored a study alongside other George Washington University researchers. The team found five biomarkers associated with higher odds of clinical deterioration and death in COVID-19 patients.

As the keynote speaker for the April 30 President’s Business Council webinar, Col. James Cummings, M.D. ’88, H’15, president of ICON Government and Public Health Solutions, Inc., discussed everything from the history of pandemics to possible vaccines.
Following his graduation from Georgetown University School of Medicine, Cummings spent 26 years in the U.S. Army. He has maintained a close connection with The University of Scranton as a member of the University’s Medical Alumni Council (MAC) and mentor to pre-medical students. Prior to his current position at ICON, he was vice president of clinical development and translational medicine at Novavax, a clinical-state biotechnology company “committed to delivering novel products to prevent a broad range of infectious diseases.”
Prior to Novavax, he was director at the Department of Defense’s Global Emerging Infection Surveillance and Response Systems (DoD-GEIS) responsible for oversight, development, functionality and fiscal accountability of the DoD’s global surveillance program for emerging infectious disease.
Here are some highlights from his talk, which you can watch in its entirety, here.
On Pre-COVID
“We’ve done a lot of learning through all of these outbreaks. And we do a lot of continued planning and learning even when there’s not an outbreak occurring. Across the whole of government, and not just the U.S. government, but other governments as well, NGOs, academic institutions, commercial biopharmaceutical companies, CROs, like the one I run at Icon, and others. We get together very regularly to discuss and learn from what we call Disease X, that’s the next pathogen, generally considered to be a viral pathogen, that will be infecting humanity and could be responsible for an outbreak or a pandemic.”
On Who it Affects
“I can tell you from the death rate…it’s not only the elderly or those who are medically compromised who are ill in the hospital, on ventilators or who are dead. This certainly has a concentration in elderly or medically compromised, but it crosses the spectrum of humanity in terms of who it’s affecting directly.”
On Biosurveillance
“There’s a national strategy for biosurveillance that’s been in place for many years. When you see a constellation of people becoming ill and you don’t know why they’re becoming ill, we’re very fortunate now that we have gene sequencing available and we can detect novel infectious agents just like this coronavirus. And that was done in China. We take that data, we review it, we integrate it, we analyze it. We turn it into actionable information that you can disseminate to key leaders and to people who can make a difference in what that information might mean. That decision gives support and feedback about where next to go for biosurveillance.”
On Healthcare Innovations
“There are DNA-based vaccines and mRNA-based vaccines. These vaccines involve injections either intramuscularly or subdermally, and then, generally speaking, some electroporation, just a fancy name for a little bit of electrical stimulus on the skin to drive that DNA or mRNA into our dendritic cells and get a robust immune response.”
“There are more traditional vaccine production methodologies either protein subunit vaccines, replicating viral vector vaccines, and virus-like particles, nonreplicating viral vectors and live attenuated virus. The inactivated, think of that like your traditional flu vaccine where we grow a bunch of virus, we kill it, then we give your immune system a little taste of that virus. Your immune system develops a robust response to that and realizes that’s the wanted poster for your immune system. The majority of these are all, for the most part, acting against the glycoprotein spike on the coronavirus.”
“There is good news on the horizon, because these platforms have already been developed for other coronaviruses. The good news is that they were able to turn the key on the machine and go very quickly with a safe product into phase one testing.”
On Cooperation
“In my short career, 26 years or so, there’s been a great development or maturation, I think, of relationships with the FDA and other regulatory agencies and industry. There are partnerships for developing solutions moving forward. Where, at one point in time, the FDA may not have been looked at as a facilitator of great products, but more of a policeman, now what’s happening is that the FDA is really bringing to bear the full might of their knowledge and their power as a regulatory agency…to ensure that we’re very rapidly assessing these investigational new drugs or vaccines or diagnostics and facilitating great work moving forward faster.”
“The regulatory process has really sped up in terms of total amount of time it requires to ensure a safe product is moving forward. That is key. You don’t want a rubber stamp, and that’s not what they’re giving. They are giving a very thoughtful review in a more expedited fashion.”
“No one’s looking for shortcuts.”
On Opening
“It’s a very fluid situation. This isn’t a light switch that we flip on and say ‘OK we’re open for business now.’ This is going to be a very segmented transition. And when you say, ‘getting back to normal,’ it’s a new normal.”
“I’m a fan of the build, measure, learn cycle. So, we’ll take a look, we’ll make a data-driven decision, then we will monitor to see what that decision produced.”
“In educators’ standpoints, there’s so much value in having people together. …You really want kids to have that socialization and that process of further maturation and development, but it can’t be at the cost of endangering their health. So I think we have to be very practical and pragmatic.”
Infectious Disease Expert Discusses Outbreaks, Responses and Covid-19
Col. James Cummings, M.D. ’88, H’15, president of ICON Government and Public Health Solutions, Inc., discusses COVID-19.

Karen Murphy, Ph.D., RN '91 is executive vice president and chief innovation officer at Geisinger and founding director of the Steele Institute for Healthcare Innovation.
In a recent interview with HealthLeaders, she discussed how Geisinger and the Institute pivoted to respond to COVID-19, from using bots to screen employees to launching efforts to do contact tracing.
Murphy was named a 2020 “Woman to Watch” in health information technology by Becker’s Hospital Review in January 2020.
Read the Q&A with her here.
Alumna CIO Discusses Innovation in the Time of COVID
In a recent interview with HealthLeaders, Karen Murphy, Ph.D., RN '91 discussed how Geisinger and the Steele Institute pivoted to respond to COVID-19.

Alex Isakov, M.D., MPH ’87 is a professor of emergency medicine and the executive director of the Office of Critical Event Preparedness and Response (CEPAR) at Emory University in Atlanta.
“Preparation for emerging special pathogens has been a large focus of my career in medicine,” he said.
In 2014, he and his team at Grady EMS, the city of Atlanta’s 911 ambulance service, transported the first person brought to the United States who was confirmed to have Ebola Virus Disease.
He was subsequently a lead contributor for the EMS Infectious Disease Playbook published by the Assistant Secretary for Preparedness and Response (ASPR) Technical Resources and Information Exchange (TRACIE).
He is now busy responding to COVID-19.
“In the early days of the pandemic, my colleagues and I recognized the need to assist the public to find guidance about their signs and symptoms of illness, and how best to seek evaluation and care," said Dr. Isakov.
They adapted SORT, a tool that they had developed and implemented for the 2009 influenza pandemic, and created c19check.com. Available for free to the public, this tool steers people to relevant CDC guidance, helps those who need emergency care to seek it immediately, and advises others with mild symptoms to seek an evaluation while maintaining social and physical distancing.
“In addition to educating the public, this tool can also provide real-time epidemiologic data that can help to identify community hotspots and inform potentially life-saving public health interventions,” said Dr. Isakov.
The tool is available in over 30 languages.
Dr. Isakov also is the Emergency Medical Services lead for the National Emerging Special Pathogens Training and Education Center (NETEC), a federally funded program that provides education, training and expert consultation to the health care community about high consequence infectious diseases like COVID-19. He contributes weekly as a panelist for the National COVID-19 Grand Rounds hosted by the Department of Health and Human Services, Assistant Secretary for Preparedness and Response.
Locally, in Atlanta, as the executive director of CEPAR, he engages daily with inter-disciplinary teams that are forging Emory University’s response to the pandemic, with “a laser focus on health and safety,” he said.
As the Director of Emory’s Section of Prehospital and Disaster Medicine in his academic department, he leads a team of emergency medicine and EMS physicians who serve the community as medical directors for 911 call centers, emergency responders and ground and air ambulances, all on the frontline of the COVID-19 pandemic.
Dr. Isakov also serves on the frontline himself, seeing patients in the Emory University Hospital Emergency Department.
“These are trying times for everyone,” Isakov said. “It’s a privilege to work with caring colleagues, skilled teams and to be part of a community that is committed to making a difference in people’s lives.”
Expert in Emerging Special Pathogens Responds to Pandemic
Alex Isakov, M.D., MPH ’87, no stranger to emerging special pathogens in his career, engages daily with inter-disciplinary teams that are forging Emory University’s response to the pandemic.

Danielle (Gilson) Healey '11 is an RN at Yale New Haven Hospital in the Perioperative Services Adult Post Anesthesia Care Unit (PACU) who tested positive for COVID-19 on April 2. Her mom, sister, niece and husband also contracted the virus.
"The University of Scranton nursing program definitely taught me to be flexible and to be ready for any situation," said Healey. "I think It has helped throughout my nine-year nursing career feel prepared and confident. I will be forever grateful for the experiences, education and the professors at Scranton."
She shared her recent experiences with us.
You got COVID-19 as more strict measures were being taken at the hospital where you work. Can you tell us what it was like at your hospital at the time?
My hospital had just started requiring employees to wear a mask at all times. Everyone was on edge and we didn't know what was going to happen with our hospital or our unit. We started training and shadowing in the ICUs to prepare for possibly floating there. Although all of the RN's in the PACU are critical care or Emergency Department trained, some nurses had never worked in an ICU or hadn't worked in one in years. Luckily I had worked in the medical ICU four years ago so I was better prepared than most of my coworkers.
We eventually would close our PACU, open as an ICU non-COVID overflow unit, and float to the various COVID ICU floors. There would eventually be four Medical COVID ICU floors in my hospital. The evening before our shift, our manager would text us saying if we were to report to the float pool or our ICU overflow unit the next day. This started happening just as I became sick, so I did not care for any COVID patients (as far as I know) before that, though looking back there may have been a couple suspected cases before we starting locking everything down.
Can you tell us what it was like to get the virus?
I was tested for COVID-19 on April 2, 2020. I started having symptoms a few days before that, which started as slight body aches. I eventually progressed to have a wide variety of symptoms, ranging from a headache behind my eyes to chills and losing my sense of taste and smell. Although I would feel like I had a fever at times my home thermometer said otherwise. I ended up losing my taste for about a month, which was very depressing as I couldn't even use food as a comfort. I developed slight respiratory symptoms about a week or so into it, which was a slight dry cough and wheeze. Luckily it never progressed to shortness of breath or anything more severe. I also had gastrointestinal symptoms at one point. All in all, it lasted about two weeks before I returned to work. My hospital's criteria was that I was symptom-free for 72 hours before returning; I did not have to test negative. Physically I was just tired throughout the whole course, mostly laying on the couch and not being very active. Mentally it was a roller coaster, because, at the same time, my mom, sister, niece and husband all got the virus as well.
Your mom and sister are nurses also nurses who tested positive. What were their experiences like?
I was extremely worried about my mom, as she is in the high-risk age group and my sister who has bad asthma. My mom had the worst symptoms of all of us. She developed a very bad cough, had fevers and severe joint aches. She was put on Z-Pack Antibiotics for possible secondary pneumonia. She and my sister both luckily avoided the hospital. My sister had similar symptoms to my mom and they also all lost their sense of taste and smell. It took my mom a month and a half to fully recover, and she just went back to work last week. I am so thankful they are all OK. It was definitely one of the scariest times of my life.
What was it like when you returned to work at the hospital?
When I returned, I cared for COVID patients who ranged from being on high amounts of oxygen on a high flow nasal cannula to being very sick on ventilators. There was such a wide variety in the ages and medical history of the patients that I soon realized COVID does not discriminate.
The whole experience was very surreal. You would arrive in the morning, stand in line to receive your PPE for the day, and then go to the charge nurse to see which floor you were assigned to. You would get a paper bag to store your masks that you reused all day and then placed in a recycling bin at the end of your shift.
I quickly realized these patients were sicker than I thought, with it being extremely difficult to wean down their oxygen requirements. There was a lot of hoping and waiting.
I tried to share my experience with the patients that I could to offer them hope and understanding. One patient I had was a very active man in his 70s who still worked and had almost no medical history. He was very frustrated and just kept looking for answers, asking me why I think this happened to him. I was at a loss for what to say to him. I just tried to make his experience as positive as I could. It made me appreciate, even more, that my family and I had mild symptoms and were able to avoid the hospital.
Can you tell us about one experience treating a COVID patient?
One of the last patients with COVID that I took care of would probably be the most memorable. She was an older woman from a nursing facility with a history of schizophrenia and dementia. She was a no-code DNR/DNI which means do not resuscitate and do not intubate, so she was on a BIPAP machine to help her breathe. She had no family or next of kin, only a legal power of attorney who made her medical decisions. The doctors caring for her painted a bleak picture in rounds that morning, talking through her plan of care but eventually realizing there was not much else they could do for her. They then talked to the medical representative about discontinuing care. When the time came, the respiratory therapist and I sat with her, and I did my best to keep her comfortable in her last moments with medication drips and pushes. I sang her a song and held her hand. I was happy that at least she wasn't alone when she passed.
How do you decompress after your days with patients?
Coming home to my husband, cat, and dog would help me decompress and let go of the day's events. My friends have also been incredibly supportive and there for me every step of the way. It helps tremendously that my mom and sister are nurses; I can talk about my stressful days and they know exactly what I'm going through.
Danielle Healey, RN '11 Returns to Work after COVID
Danielle Healy '11 is an RN at Yale New Haven Hospital in the Perioperative Services Adult Post Anesthesia Care Unit (PACU) who tested positive for COVID-19 on April 2. Her mom, sister, niece and husband also contracted the virus.

Alumni continue to respond to the pandemic. Meet some of our Royal Responders in this slideshow.
Slideshow: Meet More Royal Responders
Alumni continue to respond to the pandemic. Meet some of our Royal Responders in this slideshow.
The Panuska College of Professional Studies shares its biweekly newsletter featuring stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 29 issue here.
Here are just a few highlights from the newsletter.
Dear PCPS faculty, staff and students, especially the Class of 2020:
As you know, Mary Oliver is one of my favorite poets. “The Gardner“ by Mary Oliver reminds us all to reflect each day and to give thanks. As the spring 2020 semester is coming to a close, we remember that emergency remote learning (ERT) became our new buzz words along with Zoom, Panopto and D2L because of COVID 19. Yet, we made it! We supported each other. We became stronger together. We relaxed with music, exercise and walks in nature. Many of you will be graduating; take the time to reflect and always give gratitude. I leave you with one of my favorite songs, “What a Wonderful World” by Louis Armstrong.
Do not ever forget the colors of the rainbow.
God bless you and remember, I love you.
“Andrà tutto bene!”
Very truly yours,
Dr. Debra Pellegrino, Dean of PCPS
To the class of 2020
Grads, how you feeling’? Feeling good as Royal Here’s a song in your honor from my daughter Bethany in Dallas, Texas. She told me that you would know that the inspiration came from Lizzo. CONGRATULATIONS!
I do my cap toss,
Check my gown.
Grads, how you feelin’?
Feeling good as Royal
Cap toss
Check my gown
Grads, how you feeling’?
Feeling good as Royal
Woo Class, tired of the Covid
Go on dust your shoulders off, keep it moving
Yes, Lord, these Jesuits are off
In their jobs, careers, going to the workforce
Come now, come dry your eyes
You know you a star,
you can touch the sky
I know that it’s hard but you have to try
If you need advice let me simplify
The world is different than we thought
But know we’ve got and done a lot
I do my cap toss,
Check my gown.
Grads, how you feelin’?
Feeling good as Royal
Cap toss
Check my gown
Grads, how you feeling’?
Feeling good as Royal
Feeling good as Royal
Doctoral Degree Recipients Outstanding Graduate Student Awards
Thomas Bules – Doctor of Nursing Practice
Sophia Di Camillo – Doctor of Physical Therapy
Masters Degree Recipients Outstanding Graduate Student Awards
Geoffrey Morton – MS Clinical Mental Health Counseling
Shannon Saxon-Price – MS Rehabilitation Counseling
Christina Futterknecht – MS School Counseling
Michael Weppler – MS Curriculum and Instruction
Toni Ann Snyder – MS Educational Administration
Thomas Shaffern – MS Secondary Education
Siena Cardamone – MS Special Education
Michaela Dolde – Masters of Health Administration
Kelly Banyas – MS Health Informatics
Christine Byrd – MS Human Resources
Zachary Russell – MSN Nurse Anesthesia
Christine Pabst – MSN Family Nurse Practitioner
Mark Antonio – MSN Certified Advanced Practice Nurse
Anna Giannantonio – MS Occupational Therapy
PCPS Distinguished Graduate of the Master of Health Administration Online Program
Melissa Edwards
PCPS Newsletter: To the Class of 2020
The Panuska College of Professional Studies shares its biweekly newsletter featuring stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 29 issue here.

Eileen Parinisi Dimond '85 was part of The University of Scranton’s first graduating class of nursing students. From there, she went on to a deeply rewarding career at the National Cancer Institute (NCI) in Rockville, Maryland, where she’s been an integral part of research teams responsible for numerous innovations in the treatment of the disease.
"NCI doesn’t stop even when a pandemic hits the globe. Our mission in cancer research continues and, in fact, NCI has been tapped to use its unique resources and breadth of experience to address aspects of the pandemic," said Dimond.
She weighed on what has changed at work during the pandemic.
"While many of the cancer prevention trials I work with had to pause for accrual due to canceling of elective surgeries, research staff working from home and to limit participant exposure, the cancer treatment trials continued," she said. "It has been amazing to see everyone working together even though many of us are working from home, to do all we can to keep research moving forward."
Read The Scranton Journal profile about Dimond, before COVID-19, here.
Read more about the work NCI is doing on the NCI website www.cancer.gov or in this post about how NCI is involved in evaluating antibody tests.
Eileen Parinisi Dimond '85: The Role of National Cancer Institute During the Pandemic
"NCI doesn’t stop even when a pandemic hits the globe. Our mission in cancer research continues and, in fact, NCI has been tapped to use its unique resources and breadth of experience to address aspects of the pandemic," said Dimond.

Maura Regan ‘13 G’14, an Acute Care Occupational Therapist at NYU Langone’s Rusk Rehabilitation, is guiding COVID-19 survivors through their post-ventilator recoveries. She was named New York Post's "Hero of the Day" on May 26, 2020.
Read the story from the New York Post:
Occupational therapist teaches NYC coronavirus survivors how to walk, talk again
Maura Regan ‘13 G’14 Named New York Post's Hero of the Day
Maura Regan ‘13 G’14, an Acute Care Occupational Therapist at NYU Langone’s Rusk Rehabilitation, is guiding COVID-19 survivors through their post-ventilator recoveries. She was named New York Post's "Hero of the Day" on May 26, 2020.

While most are keeping their distance during the pandemic, three Scranton alumnae remain in close proximity to one another in New York City.
Mary Rose Ho '10 and Liz Waldron Capobianco '01 are nurse educators at NYU Langone, responsible for the education of nurses entering the health system as well as the ongoing education needs of all the nurses at NYU. As the first stop for new nurses, the two often meet Scranton alumni as they begin their new jobs.
"It is a special connection, and I think it is comforting for us, as well as the nurses new to NYU," said Capobianco.
In April, they welcomed one recent alumna to NYU: Lauren Garel ‘17. Once Ho found out she was a Scranton graduate, she shared the news with Capobianco, and they quickly connected with her.
"She started her first nursing job at the height of the pandemic here in New York, which has been a most difficult and frightening time," said Capobianco. "As we would expect from a fellow Royal, Lauren has handled herself with poise and grace during this uncertain time."
Ho and Capobianco have worked in the Department of Nursing Professional Practice as Nursing Professional Development Specialists for about two years. In just two weeks during the pandemic, they "have educated an increased number of nurses new to NYU as well as 400+ travel RNs."
They have also trained existing nurses that work in perioperative and procedural settings to the inpatient setting and over 200 acute care nurses to care for ICU-level patients as NYU opened more ICU’s to meet the need of the COVID-positive patient population.
Garel and Capobianco helped discharge the 1,000th COVID patient from the hospital when Capobianco suddenly recognized an attending physician in the crowd, Dr. Kevin Huack '07.
"I introduced him to Lauren, and said, 'Look at us Scranton grads at this historic moment!'" said Capobianco. "I then had the honor of helping to escort the 1,000th COVID patient out of the hospital to the cheers of hundreds of our employees and watched her reunite with her daughter who she had not seen for a month while she was in the hospital. There was not a dry eye in the crowd, and I was so honored to be a part of it."
The Scranton alumnae continue to reach out to new nurses who enter the NYU system.
"It is always fun to connect with them and reignite our Scranton community here," said Capobianco, who met one of her best friends, also a Scranton grad, at NYU. "I think Scranton grads gravitate to each other and also gravitate to the greatest challenges, which is why I am so proudly with so many right now."
One she can no longer be with is her former NYU colleague and Scranton classmate, Mary Grace Dirks '01, who recently died of cancer at the end of April. Because of the pandemic, no visitors other than Dirks' husband, also a Scranton alumnus, were allowed to visit her. Just hours before she died, a mutual NYU friend was able to hold Dirks' hand and "tell her that all of her Scranton friends loved her," said Capobianco.
"The nursing world is strong and loyal," she said. "Scranton built a sense of community that is unlike other universities."
Nursing Alumnae Connect at One NYC Hospital
While most are keeping their distance during the pandemic, three Scranton alumnae remain in close proximity to one another in New York City.

The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 15 issue here.
Here are just a few highlights from the newsletter.
My dear PCPS friends,
David Denotaris, who has been a speaker at our University’s Conference on disABILITY is one of my favorite motivational speakers. He often speaks about faith, family and friends. He’s also been known to reference the beloved Mister Rogers who encourages young people to “Look for the helpers” in life.
That got me thinking. Yes, we need to look for the helpers. But maybe there are times when we need to do even more. A few years ago, I read Ian Bogost’s article in The Atlantic (Oct. 29, 2018) where he discussed that looking for helpers is insufficient at least for adults. As adults, he says, we might take away the wrong lesson from this quote.
For adults, there’s a slightly different twist on Mister Rogers’ famous words. We must BE the helpers. In a world that has been turned upside down by the effects of COVID-19, we, as adults, need to BE the helpers that young people turn to when they are looking for the helpers.
In this issue of our e-newsletter, Call to Care, you will see even more examples of how PCPS undergrad and grad students, faculty and staff, are heeding the call to BE helpers in the spirit of St. Ignatius, founder of the Jesuits.
Very truly yours,
Dr. Debra Pellegrino, Dean of PCPS
OT Portfolio Day
Held On Friday, May 8, 2020, the Occupational Therapy Graduate Portfolio Day was held via Zoom. There were several 'tables' that included six students and Occupational Therapy faculty. The graduate students shared their most significant experiences during their five or six years. Dr. Carol Coté, Chair of Occupational Therapy, arranged sessions at 9:00 a.m. and 2:00 p.m.
Faculty, families and friends were invited to the nine zoom sessions. It was fabulous to see the evidence of outcomes in leadership, ethics, the Jesuit mission, and service, to name a few objectives.
Music to Get Us Through Finals
Emma Reed, a Secondary Education major with an English concentration from the Class of 2022, sent an email last week to reach out to PCPS students who are preparing for finals. Here is her note.
“I hope you are doing well! I just wanted to send a quick email to you and thank you for your emails. They really do brighten my day and give me hope. I am so proud and happy to be a part of PCPS. It is people like you that remind me why I want to be an educator and woman for others. If there were any education I would want to have it’s a Jesuit education, especially from The University of Scranton.
"There are two songs that I wanted to share with you that I believe would benefit our Scranton community. I always listen to these songs when I am down and need a little push. They truly give me hope and remind me that eventually, things will be ok. One of these songs, "Almost Everything" has a lyric that always pushes me forward: 'It feels bad now but it's gonna get better.'
Artist: Wakey!Wakey!
I hope that these songs inspire you as much as they inspire me and that you share them with my fellow PCPS students. Stay well and inspired!”
PCPS Newsletter: 'Be the Helpers, Look for the Helpers'
The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 15 issue here.
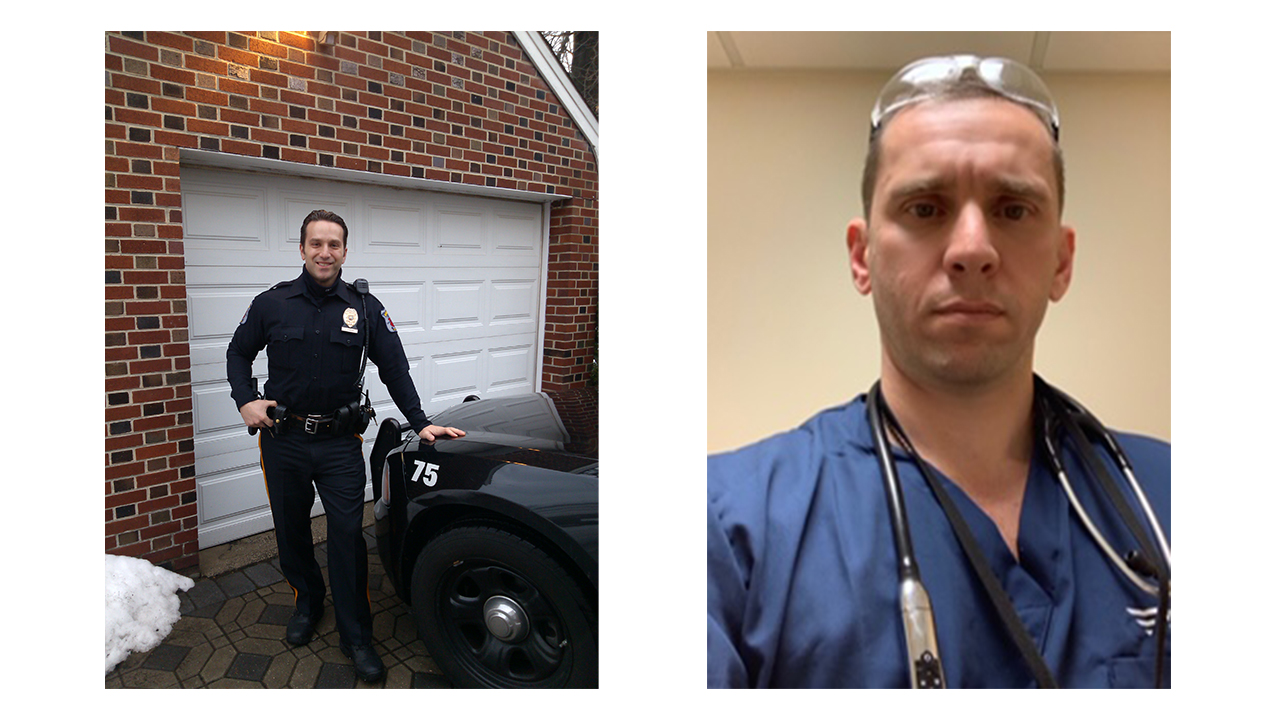
Freshman year roommates James Kompany '95 and Vince Carsillo '95 don't get to see each other often, but they were both looking forward to reconnecting at Reunion this year, a break from their demanding jobs in law enforcement and health care. Instead, Reunion has been postponed and they're both navigating unfamiliar territory during the pandemic. Kompany is a police officer in Roselle Park, New Jersey, and Carsillo is a physician whose internal medicine and nephrology practice in Albany, New York, is taking in COVID patients from New York City.
"Personally, I am taking the same precautions as most of the rest of society in order to stay healthy and safe. Like so many others, I have been forced to alter my lifestyle until this crisis is behind us," said Kompany, a 17-year veteran of the police force, currently a corporal in the patrol division.
At work, Kompany and his fellow officers wear protective gear when interacting with the public and respond to many non-emergency calls in what would be considered a highly unusual way during normal times, via phone rather than patrol car.
As Kompany is receding from the frontlines in some ways, Carsillo is advancing toward the frontlines as his team takes on COVID-19 patients.
"My group provided care to those patients and many required ICU care and acute dialysis related to the virus," said Carsillo. "In the outpatient setting, we needed to reorganize our dialysis units so that we could care for the infected patients at one isolation unit. Personally I am happy that we have seen a decrease in cases and proud of the job my group and my colleagues have done treating the sick and navigating this new medical challenge."
Carsillo is also proud of his former roommate and good friend.
"I have great respect for our police and the work that Jim and his colleagues do every day to protect the public," he said.
They both credit The University of Scranton for helping them through this difficult time.
"My preparedness comes through faith in God," said Kompany. "And this faith was solidified during my time at The 'U.'"
Carsillo agreed.
"Scranton surely prepared me to manage this crisis. I learned that you can find joy in the service of others and, in the words of Thomas Aquinas, that 'there is nothing on this earth more to be prized than true friendship,'" he said.
Kompany and Carsillo both said that they'll miss seeing each other during Reunion this year, but they appreciate one another more than ever.
"When [Vince and I] connect, we constantly laugh at the same stories and can easily pick up where we left off on our last conversation," said Kompany. "I'm proud to call him a lifelong friend."
Reunion is Postponed. Friendship is not Canceled.
Freshman year roommates James Kompany '95 and Dr. Vince Carsillo '95, who are both navigating unfamiliar territory during the pandemic, will miss reconnecting this summer at Reunion. But they are reminded of what Scranton gave them.

 It's Nurses Day. We value the hard work of our RoyalRNs every day, but today, this year, we want to send them a special thank you. We have gathered some of our recent Royals Respond stories featuring nurses, and those who support them, below.
It's Nurses Day. We value the hard work of our RoyalRNs every day, but today, this year, we want to send them a special thank you. We have gathered some of our recent Royals Respond stories featuring nurses, and those who support them, below.
We continue to honor them, and other health care workers, each evening when we light St. Thomas Gateway with a red cross, which you can read about here.
You can browse through our Honor Roll, which honors Royals on the frontlines, including 159 nurses, here.
Taylor Kerrane '16: Brother Pays Tribute

Conor Kerrane '12 writes a tribute to his sister, Taylor Kerrane '16, an ER nurse for Northwell Health in Long Island, New York.
Taylor Kerrane '16 graduated at the top of her class from The University of Scranton with a BS in Nursing. She chose this career path as it compliments her caring nature and ambition to bring good health and faith to the world.
Early in life, Taylor succeeded at many things and, after graduating, was propelled by her education into a great career as an ER nurse for Northwell Health in Long Island, New York. She was selected from hundreds of other graduates across the nation into a high-profile program at Northwell to train with best-of-breed professionals and cater to a high demand, high-stress environment.
With her training and drive, Taylor has stepped up to the plate to address the COVID19 outbreak alongside her colleagues with world-class professionalism and bravery. She has endured the stress of helping over 100 COVID19 positive patients in her hospital and continuously fights on the line to save lives.
Read the entire story here.
Isabella Dolente '17 is Honored by her Parents
Isabella Dolente '17 is a nurse who is working to combat COVID-19 in Philadelphia. Her parents, small business owners Carl and Lisa Dolente P'17, P'23 from Haddon Heights, New Jersey, were so proud of their daughter on the front line of the pandemic that they made shirts that say, "Not All Heroes Wear Capes. My Daughter Wears Scrubs." The saying was sent to them from Scranton staff member Lynn King Andres '89, P'17, director of the Parents' Executive Council (PEC). The couple, members of the PEC, sent the T-shirts to the family and friends of Isabella's nurse colleagues. Their daughter, Miranda, is a first-year student at Scranton.
Isabella responded to her parents' generosity by posting a thank you on her Facebook page, "Before all this, I can say that I’d taken my parents hugs and kisses for granted. I have not missed something more. Thank you for being the two best humans I know. The strongest and greatest support system a daughter/nurse could have."
Read the entire story here.
Thank you, nurses!
Tell us how Royals you know are responding during this crisis.
Share a Story
The University community is invited to share individual stories, photos with captions, news coverage, video footage or reflections that may be featured on the Royals Respond section of the Royal News website and shared in social media and other University publications in the weeks and months ahead.
Click here to share a story.
Honor a Royal
We also invite students, faculty, staff, alumni, parents and friends to recognize someone connected to the University who is helping the nation and the world respond to the pandemic. Submissions will be gathered in a Royals Respond Honor Roll which will be shared on this page, and on the Royal News website.
Click here to Honor a Royal.
Nurses Day: Collection of Stories
It's Nurses Day. We value the hard work of our RoyalRNs every day, but today, this year, we want to send them a special thank you. We have gathered some of our recent Royals Respond stories featuring nurses below.

The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 1 issue here.
Here are just a few highlights from the newsletter.
Join the Love Letter Link or the Rainbow Hunt
Gerianne Barber, Director of our Counselor Training Center in the Department of Counseling and Human Services, sent this email out to her family and friends, inviting them to join the Rainbow and Love Letter Link Initiatives at the Jewish Home, where her Mom is a resident.
TO MY FAMILY AND FRIENDS I wanted to let you know that the Jewish Home has started two initiatives.
One is called the LOVE LETTER LINK. Essentially, they are asking that we send pictures and cards to our family members to “flood” their rooms and the home with cheer. If you are able, please send a card or note to my mom. I know she would enjoy it and I would be grateful for your help. The home will share the cards and notes and use them to decorate the rooms of residents! This will surely boost their moods and help add joy for both the residents and the staff. There are some residents who may not have family, so cards and notes for them would be wonderful as well. There are several options for safely sending/delivering these to the Jewish Home.
• Feel free to mail them through the US Postal Service. We are able to then receive them safely and deliver them safely. Address is: Mary Grace Barber C/O Jewish Home of Eastern, PA 1101 Vine Street, Scranton PA 18510
• Email your notes to: Nicole Lipinski @ nlipinski@jhep.org. She will print out letters and even pictures on a color printer, and then we’ll get them to my mom.
Ever since I was a little girl, my mom always told me that a rainbow was just an upside-down smile. Without a doubt, I still chase those rainbows and always have hope when I see one. As the ugly Beast started to appear in Europe, we saw the Italian people singing from their balconies and posting banners, paintings and drawings with rainbows that included the message “Tutto andrà bene.” That translates to “Everything will turn out OK.” As COVID-19 began to make its way across Europe, we then started to notice those same rainbows appearing in people’s windows in Canada, and through the United States. Rainbows were everywhere and could be found in New York City and Philadelphia. Now, there is a call for rainbows to appear in Scranton, Pennsylvania. In a recent article by Chaunie Brusie, she stated, “If there’s one thing that we always look for after a storm, it’s rainbows. Those unexpected color bursts through the sky never fail to bring us running outside to look up with a smile on our faces.” In another article, Lee Ann Jones, an ICU nurse from Florida, told a Florida news station that she believed rainbows symbolize hope and we need it right now because we need hope because this virus COVID-19 is very scary. Jones told the news station that her sister in New York actually inspired her to start the Rainbow Hunt group—and the rest has been history. Now, her original 904 Rainbow Hunt group on Facebook has over 5,600 members, with new members joining every day, and many on social media are sharing their own #RainbowHunt finds too.
Long Hours on the Frontlines
 Patrick Nancoz ’21, an Exercise Science major, is currently working as an EMT for the West Essex First Aid Squad in West Caldwell, NJ.
Patrick Nancoz ’21, an Exercise Science major, is currently working as an EMT for the West Essex First Aid Squad in West Caldwell, NJ.
“We are in a harder hit region due to COVID-19. With our call count tripled, several of our college members have been on call for large numbers of hours,” he said.
Patrick was on call for about 80 hours this past week, as was his Scranton housemate and partner on the squad, Thomas Salandra ’21.
”Our main roles have been patient care and transport to area hospitals, with the majority of our calls being for elderly patients with either suspected or confirmed COVID-19," he said.
Drop-in Nclex Review for Senior Nursing Students
Thanks to Dr. Sharon Hudacek, RN, ACNS-BC and the wonderful nursing faculty for taking hours of their valued time to design ten “Drop in Review“ sessions for our nursing seniors. These sessions have been very well attended and received by our seniors who are preparing each week for the new, abbreviated form of NCLEX (through July 4). The senior nursing students soon will finish Phase 1 of the Kaplan Study Recommendations. Thanks, also, to Dawn Mazurik for scheduling these valuable zoom meetings for our seniors – the future Royal RNs!
With a Little Help from my Friends
 Anthony F. Carusotto, D.P.T., an instructor in the Physical Therapy department, invited all of our DPT Year 1 students to a Zoom Talent Show. He hosted the event, and at least a dozen of the students showed off some of their talents — cello playing, singing, guitar playing, and soccer ball dribbling, among other things. From his own home in Dallas, Pennsylvania, he created a tune on his guitar. According to Dr. Renée Hakim, chairperson, they are now planning to have a bigger talent show on Cinco de Mayo for all DPT students (Years 1, 2 and 3), as well as the new incoming student group.
Anthony F. Carusotto, D.P.T., an instructor in the Physical Therapy department, invited all of our DPT Year 1 students to a Zoom Talent Show. He hosted the event, and at least a dozen of the students showed off some of their talents — cello playing, singing, guitar playing, and soccer ball dribbling, among other things. From his own home in Dallas, Pennsylvania, he created a tune on his guitar. According to Dr. Renée Hakim, chairperson, they are now planning to have a bigger talent show on Cinco de Mayo for all DPT students (Years 1, 2 and 3), as well as the new incoming student group.
PCPS Community Comes Together
The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire May 1 issue here.

In mid-March, Alyssa Muchisky '16, a medical student at the Geisinger Commonwealth School of Medicine, and many other third and fourth-year medical students around the country were pulled from their clinical rotations due to the lack of personal protective equipment.
"We knew the strain this pandemic would put on our country's hospital systems, and we felt powerless because we could not help our colleagues on the frontlines," she recounted. "A bunch of third-year students got together and brainstormed ways we could support our hospitals from afar, and that is when we came up with the idea of Meals for Medics."
The group of students, along with Scranton Tomorrow, founded Meals for Medics, which raises money to buy hot meals from local restaurants for health care workers at Geisinger Community Medical Center. They are delivered to the hospital by the medical students. On April 23, they delivered more than 300 meals to third shift staff who work at night.
"All of us have worked shifts in the hospitals that are hectic and unpredictable. Sometimes hospital workers have as little as five minutes to quickly eat before moving on to the next task," said Muchisky. "We wanted to provide readily available nutritious options for all hospital staff during this time."
Muchisky, a Scranton native, is glad to be able to help her community during the pandemic.
"This project is really near and dear to me because its a small way I can give back to a community that has already done so much for me," she said.
Alumna Establishes Meals for Medics in Scranton
Alyssa Muchisky '16, a medical school student, established Meals for Medics to donate hot meals to local health care workers.

In early March 2020, a cruise ship carrying passengers afflicted with COVID-19 docked in Oakland, California, and many of the patients were sent to the hospital where Liz Durkin, M.D. ’93 works as a palliative medicine physician.
“These patients were fortunately not critically ill, but we were aware early of the challenges for staffing and PPE [personal protective equipment] in caring for COVID-positive patients,” said Durkin, who works at Permanente Medical Group in northern California. “Our palliative hospital teams have been working on preparedness for a possible surge in cases for the last two months, including new workflows relying on virtual visits, even with hospitalized patients, to minimize the need for PPE in the room. We have also been working on educating other physicians and team members on how to care for patients at the end of life in a compassionate and dignified manner.”
As the COVID-19 pandemic has spread across the United States, Scranton palliative care physicians and nurses are a vital part of caring for patients and supporting their families in isolating circumstances. Both in Scranton and on the West Coast, Royals in palliative care are using technology to maintain connections among patients, families and care teams. And they have been bolstered by community support in times that are unnerving for patients, families and health care workers alike.
Palliative care is not the same as hospice care, which begins after treatment for a disease concludes. While both these methods aim to keep patients comfortable, palliative care is for anyone with a serious or chronic illness and is best begun at diagnosis. Palliative care physicians and nurses, working with specialists who provide curative treatments, help patients understand their choices for medical treatment and recommend treatments that can help control symptoms and improve quality of life.
“In palliative medicine, our goal is to make sure that we are inclusive of all of a patients’ beloveds, which usually includes meeting them in person and having large family meetings to discuss the plan of care for a patient,” said Lauren Nicholls, M.D. ’11, who works at Geisinger Community Medical Center in Scranton. “We make it a priority to break down any barriers between families and the medical team.”
Patricia Wright, Ph.D., a University of Scranton nursing professor, said that palliative care is especially important for patients with COVID-19, since there is no immediate cure and it is life-threatening for some patients.
“Palliative care is often incorporated into the treatment of chronic conditions, but it becomes even more important when a disease is potentially life-threatening,” said Wright, who specializes in community health and hospice care. “In cases of COVID-19, the challenge is to hope for the best while preparing for the worst, meaning that even patients with mild symptoms should be invited to develop an advance care plan in the event that their condition rapidly worsens.”
Working with patients and family members to do just that has become more challenging during the pandemic, according to Nicholls. Her hospital has a no visitors policy in place, unless patients are dying. But patients dying of COVID-19 are not allowed visitors for fear of passing on the disease to family members.
“Now, in addition to the physical barrier of distance between us and the family, we have the physical barrier of the PPE between us and the patients,” Nicholls said. “The entire manner in which I typically connect with families has been disrupted. To make up for the lack of physical contact with patients and families, I have been relying on the telephone far more and making sure to relay the little things, such as get-well cards made by local children for our ICU patients, to let families know that their loved ones are not just another name in a bed; they are a whole person, being loved by our team in their absence.”
In Oakland, Durkin is employing similar phone and video communication methods with patients’ families, especially elderly patients who are without their usual support systems in hospitals with restricted visitor policies. Here in Scranton, Laura (Pikulski) Marion ’92 is the assistant vice president of Allied Services Hospice and Palliative Programs in Scranton, and she is working with patients in their homes, nursing homes, or the organization’s hospice care center. She’s helped implement telemedicine virtual appointments for patients and helps them stay connected to their families with video calls instead of in-person visits.
“We’re rewriting policies almost daily as things change so quickly with the Department of Health and the CDC. Some days trying to manage, learn, read, and share all the information is exhausting, and the days are long and I tend to be weary,” said Marion. “Loved ones aren't seeing their family for two to three weeks, elderly are isolated and no one is immune. Healthy people are being stricken by this virus. This is not hype; this is real and it is highly contagious.”
Durkin shared Marion’s concern for the elderly and isolated patients, as well as the health care workers treating them.
“I think the hardest part of this is the unknown,” said Durkin. “I am vulnerable to this infection, and even otherwise healthy individuals may have poor outcomes when faced with this disease. We are usually able to have the perspective of ‘distance’ from our patient's illness, but not in this case. We are all vulnerable.”
Even in the face of fear and unknown, Marion said people in the Scranton community are rallying to support both patients and health care workers.
“Folks reaching out to offer to make homemade masks and donate, local restaurants offering to feed our nurses and staff, donations of food being dropped to the hospice center,” Marion said. “There are folks offering to sit and make phone calls to our home patients to make sure they are not isolated. Amazing things are coming out of this on a daily basis.”
‘We are all Vulnerable’: Palliative Care during COVID
Palliative care doctors and administrators use technology and community support to help patients and their families.

Now more than ever, it feels extra special to hear a familiar voice.
In a time where staying distant is the new normal, our emotions can get the best of us. In a school community that feels like home to most, students and staff alike are starting to feel homesick. It is difficult to comprehend the state we’re living in right now, and it is reassuring to know that our tight-knit University will do whatever it takes to keep our spirits high.
Through this pandemic, the University has found ways to be more connected than most of us ever thought possible. Whether it’s the transparency of Father Pilarz’s emails, the Remote Royals updates each week, or simply spending a few hours sharing laughs with friends over Zoom, the University community found ways to reach out to our fellow Royals.
But, more recently, a handful of staff members took an extra step in keeping us connected. Two weeks ago, Fr. Pilarz notified students that he had asked staff to make calls to students to check-in and see how we were doing. I caught up with a few University staff and students to reflect on the calls and what it felt to hear the voices of those we might usually see walking around campus.

Maria Marinucci (pictured at left), director of the Cross Cultural Centers, reflected on meeting new students, the positive attitudes during this challenging time, and hearing the experiences of those who had been sent home from studying abroad.
“I really enjoyed making calls to students this week; in fact, it was one of the highlights of being a remote Royal for me!” Said Marinucci. “I didn’t know any of the students on my list, so getting to connect with new students is always exciting and at times confronting boredom in different ways as well.”
She found that students were feeling challenged, yet supported.
“Each student with whom I spoke was really positive, even while discussing personal and academic challenges,” she said. “Without fail, each student shared how many of their faculty members were being really supportive, and they acknowledged knowing we all were navigating something completely new together and they described a sense of togetherness even in isolation.”
 Grace Okrepkie (pictured at left) is an occupational therapy first-year at the University. She is one student who feels the “togetherness” that Marinucci described.
Grace Okrepkie (pictured at left) is an occupational therapy first-year at the University. She is one student who feels the “togetherness” that Marinucci described.
“Everyone is scared during this time of uncertainty, so it is comforting to know the University cares about the well-being of its students,” she said. “As a first-year, I just recently decided to attend here mostly because it was heavily emphasized that this community feels like a family. This has proven to be true, considering the staff has generously decided to check in on each of the students.”
The calls turned out to help staff feel connected as well, said Marinucci.
“We were able to empathize with one another about general uncertainty and stress, as well as the difficulties of focusing on school or work at home and navigating competing demands, gotten sent home from a semester abroad, which was just a new level of disappointment,” she said.
The students that Marinucci talked to were “upbeat and understanding,” she said. “I found that so motivating and inspiring.”
They told her how they were connecting via Zoom to study, play trivia and just talk.
“It reminded me how even in the toughest of times when we reach out to one another, we can often find strength, encouragement, motivation and connection. And it also made me even more grateful for our Scranton community!” she said. “I can only hope the students felt as uplifted by me as I did by them.”

Toby Lovecchio (pictured at left), who serves as chief of staff to Fr. Pilarz, made calls to graduate students, and some of the students, he said, were surprised to hear a real person’s voice. One student anticipated a pre-recorded check-in and was “just so happy to hear [his] voice.”
Lovecchio said out of the 40 students he called, he was able to speak to about a third of those, and the majority of students said they were glad to get spiritual messages from the University.
“It’s a cool idea, it says a lot about who we are,” said Lovecchio.
 Matthew Marcotte (pictured at left), a junior forensic accounting student at the University, found that the check-ins a reflection of the strength of this community.
Matthew Marcotte (pictured at left), a junior forensic accounting student at the University, found that the check-ins a reflection of the strength of this community.
It’s “a really good representation of how supportive the Scranton community is,” said Marcotte. “It was an effective way for students to understand that they’re not alone; there are people who care about them, and we’ll all get through this together.”
Okrepkie agreed.
“The dedication goes above and beyond, thus making me proud to be a Royal!” she said.
Staff or student, the check-in calls prove that even if we might be many miles away from one another, we are still close. We will get through this difficult time, “for and with others,” just as Royals do.
Staff ‘Check-in' Calls Show Strength of Community
Abigail Corrigan ’21 reports on how staff "check-in" calls reflect the strength of the University community.

Hear from Kelly Sarti Wroblewski ‘02, director of infectious disease programs for the Association of Public Health Laboratories, about the COVID-19 testing landscape.
WHO: Kelly Sarti Wroblewski ‘02, director of infectious disease programs for the Association of Public Health Laboratories
MAJOR: Medical Technology
ADDITIONAL EDUCATION: Master of Public Health at Johns Hopkins University
HOMETOWN: Moosic, PA
CURRENT CITY OF RESIDENCE: Silver Spring, MD
FAMILY: Husband, Ed, and sons, Eddie, 8, and Calvin, 4
Kelly Wroblewski’s role in the pandemic response can be likened to that of a detective in a war zone. As a director in a public health network, she’s worked both quietly behind the scenes yet vocally on the frontlines. Her primary weapon has become the holy grail in this battle: the long-awaited COVID-19 test.
Wroblewski’s daily tasks differ from those of other scientific groups responding to a public health emergency. Public health laboratories, present in every state, monitor the collective health of the public and inform the care of the population rather than the individual. An organizational leader in the national network of public health labs, all of which were on high alert awaiting from the CDC the assay, or chemicals, that would detect the virus, Wroblewski and her crew have been first responders in another sense of the word. That’s because, in the early days of the virus, only public health labs were allowed to run testing. She became a vanguard, however, in getting all critically needed hands on deck.
Having begun her career at a microbiology lab at a small Pennsylvania hospital before taking a fellowship at the National Institutes of Health working on antimicrobial resistance then earning her MPH and working in the clinical lab at Johns Hopkins, Wroblewski has participated in many outbreak responses. So while COVID-19 is a novel virus it’s familiar ground for her.
She kicked her leadership into high gear after Jan. 18, the day on which the CDC detected the first case of the virus in the United States. Much of her role then was to work the phones furiously, assessing whether individual laboratories were ready with the necessary supplies and equipment once the assay was released and the labs could then “test the test,” so to speak, before themselves administering it.
Because of the now-well-known problems with the first released test and the initial prohibition on private labs doing testing, Wroblewski made an unprecedented move as the country awaited some positive news: She wrote to the FDA asking for permission for public health labs to make their own tests.
Because the first case in the United States with untraceable origins confirmed that COVID-19 had taken root here, the FDA essentially agreed, permitting advanced labs to develop their own tests.
This was a watershed moment for public health laboratories, and Wroblewski was at the forefront.
Royal News (RN): Kelly, it can be said that you are working in an epicenter of the fight against COVID-19. You recently told NPR that the situation with testing in America was “a giant mess” but that you were trying to remain optimistic that there was a light at the end of the tunnel. In the few weeks since you’ve spoken to NPR has the availability and effectiveness of the rapid test increased your optimism on the testing front?
Kelly Wroblewski (KW): The rapid molecular test is certainly another welcome tool in the toolbox, but, like many other testing supplies, there are limits to the availability of reagents, and it is not going to be the best fit for every setting. We continue to increase and improve capacity, but we still have room to improve both in terms of testing capacity and testing strategy. We are making progress, though.
RN: Early on, just after the virus hit the United States, the initial test fast-tracked by the FDA was considered glitchy at best, and it wasn’t until late February that a new test finally showed up. Can you tell us a little more about the mood in your sector during those waiting days?
KW: There was definitely an anxious vibe. We roll out and implement new tests with some frequency, and this had never happened. So there was a certain amount of disbelief and a lot of anxiousness as the public health laboratories waited for some resolution to the problem.
RN: Are the right people able to receive access to the rapid test right now? And, if not, who are the right people who should be receiving access?
KW: The rapid test has opened up testing, but it’s by far not accounting for the bulk of the tests being performed. The rapid test is really best used in settings where a there isn’t easy access to laboratory testing and a fast result is needed to inform decision making. Examples include places like rural critical access hospitals, nursing homes or prisons.
RN: What needs to change right now when it comes to testing?
KW: We need a high-quality, well-vetted antibody test. More than that, we need a thoughtful, feasible testing strategy that includes implementation details. Up to this point we’ve been so reactionary; we’ve been reacting to a new problem every day. We need to take the time to build plans with some scientific rigor behind them.

RN: Can you describe your emotions after you essentially got the ball rolling with the FDA so that public health labs could work independently on their own tests? We’d love to hear of your excitement as well as your fears.
KW: A few things happened at once. As they opened up the pathway for laboratories to develop their own SARS-CoV-2 tests, FDA and CDC also dropped the problematic component of the original CDC test. So in the end, most of the public health laboratories moved ahead with the CDC assay. My primary thought at the time was pushing to make sure public health labs brought a test on as expeditiously as possible. It was exciting to be involved in shaping policy in that way. I really look forward to the after action and thinking through how we use some of these actions to build a system that allows us to do better in the future.
RN: The testing landscape – at least in terms of who was allowed on the mat – essentially went from public health laboratories flying solo to private laboratories and eventually the private sector all contributing. What’s the next best step in this battle – for everyone involved in testing?
KW: We are going to need all hands on deck for a long time. It goes to what I said before about developing a thoughtful strategy. All of those laboratories from point-of-care testing sites to hospital labs to commercial labs to public health labs have a role they are best suited to play. Defining those roles and ironing out the logistics of getting the right specimens to the right labs is going to be key to ensuring we are using all of our laboratory resources most efficiently. It will be a critical component of this next phase.
RN: Is this the fight of your life so far? Can you tell us how your Scranton education armed you for it?
KW: Someday, I am sure it will all sink in and I will feel that way. Really though, I’ve been taking it one day at a time, addressing the problem in front of me to the best of my ability and moving on to the next one. Scranton, for me, struck that perfect balance between being challenging and supportive. I never felt coddled and worked really hard. At the same time, I felt that my professors wanted the very best for me and therefore expected the very best effort out of me. It’s that sense that putting forward your best effort is going to yield good results.
Ask the Expert: Kelly Sarti Wroblewski ‘02
Hear from Kelly Sarti Wroblewski ‘02, director of infectious disease programs for the Association of Public Health Laboratories, about the COVID-19 testing landscape.

Maria Vital G’11, operations manager of the Leahy Clinic, thanks health care providers.
You can thank Royal Responders as well! Visit scranton.edu/royalsrespond to honor a royal or share a story. To thank a member or friend of the Scranton community helping the fight against COVID-19 via video, click here.
Video: Maria Vital G’11 Thanks Health Care Providers
Maria Vital G’11, operations manager of the Leahy Clinic, thanks health care providers.

The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire April 17 issue here.
Here are just a few highlights from the newsletter.
School Counselor Develops Online Resources for Students
Jacqueline Bailey | BS CHS 2017 | MS School Counseling 2019 | Certificate of Advanced Graduate Study (CAGS) Spring 2020 | Hometown: Old Forge, PA
Jackie Bailey became the first school counselor at The Scranton School for Deaf and Hard of Hearing Children in August 2019. When the pandemic closed the school facility, Jackie had just one week to prepare her online materials and resources.
Here’s what is featured in the online materials that she assembled:
• Resources for families – providing information on access to food, internet resources, mental health resources, and health care resources
• Resources to help parents – especially how to talk to their children about what is going on in the world
• Resources for the social-emotional learning class that she teaches. There are assignments for students, families and parents /guardians /caregivers
• The class still meets regularly online, and Jackie invites other staff (custodians, cafeteria staff, office staff, administrators) of the school to “drop-in” and say “Hi” to students
• Jackie developed multiple ways for students in her class to contact her: º Students check-in and leave mail, telling how they are feeling and what is going on (picture-based so it is accessible for youngest students) º Parents email what is going on in-home and request family counseling or counseling with student º Virtual office hours, including a doxy.me waiting room where students/parents can have a confidential session
• A virtual staff lounge where staff can post ideas, events that motivate them or ask questions
• Therapy dog corner featuring pictures of Jackie’s very own therapy dog and an opportunity for students to “ask questions” to the dog
• Deaf community resources
Feedback on Transition to Online Learning
 Kim Subasic, Ph.D., MS, RN, CNE, interim chair of the Department of Nursing, has been hosting virtual coffee chats with the student nursing representatives in each cohort.
Kim Subasic, Ph.D., MS, RN, CNE, interim chair of the Department of Nursing, has been hosting virtual coffee chats with the student nursing representatives in each cohort.
“Three of our nursing student representatives recently participated in a virtual faculty meeting. All three reported feeling good about the learning and the quick adoption by the professors and the University to new learning modalities for the students. They expressed thanks to the professors and that, despite the changes in learning, we are still continuing to hold the extra things we do, such as the Kaplan review sessions for seniors. Students reported that they like the variety of teaching methods we instituted despite the steep learning curve. For the most part, the students also feel as though the transition to remote learning hasn’t been too bad.”
'Don't Stop Believing'
Amy E. Russell | Graduate Student | Health Administration Program
During a routine shift at a hospital in Westbrookville, New York, Amy experienced both the clinical and human faces of the COVID-19 pandemic. “It is like nothing I have ever seen or could have imagined,” she says. “People working in the ER in full gear …an N95 with a regular fluid mask over that, face shield, gowned and gloved."
Then something happened that caused everyone to freeze in their tracks. "The song Don’t Stop Believing" by Journey came over the PA system. We were told that every time someone recovers from COVID and is discharged they play that song to spread a little joy. I was blessed to hear it five times during my shift,” says Amy.
She went on to note the “unsung heroes” of the hospital – the environmental services staff who are cleaning and trying to keep everyone safe with only limited protective gear.
"I chose to work in health care, I am hoping we hit our peak soon and can start to recover. I think this is further out than many realize; I also worry about the reduction in the workforce because of lost profits," she says. "I want to thank the professors for being understanding in these uncertain times. For those called to serve on the frontlines, I pray they stay safe and healthy. I also pray for the safety and health of the families of those on the frontlines."
'We can get through this together'
Caitlin Thompson | PT | Class of 2015 | Hometown: Wantagh, NY
Caitlyn, a physical therapist at New York LIJ Health care system, took to Facebook to extend a special invitation to friends. Her post made it to the Geisinger Wyoming Valley Health Care System in Wilkes-Barre per Chandra Dombroski Nealon, a faculty specialist in the Occupational Therapy Department. “If you have a family member or loved one who is hospitalized, I would love to stop by and see them before or after my shift ends. I can FaceTime them for you or offer well wishes. "If you want to go fast, go alone. If you want to go far, go together. We are stronger together and we can get through this TOGETHER.”
PCPS Students, Faculty and Alumni Respond
The Panuska College of Professional Studies has created a biweekly newsletter to share the stories of those who answer the "call to care" during the COVID-19 crisis. You can read the entire April 17 issue here.

Colonel (R) Richard H. Breen, Jr. ’77, past president of the University's Alumni Society Advisory Board, is the director of Strategic Communications for the Military Health System (MHS), Department of Defense, at the Pentagon. In this capacity, he directly supports the assistant secretary of defense for Health Affairs and the director of the Defense Health Agency in all aspects of Military Health communications. He is coordinating all the military medical communications activities for the MHS during the COVID-19 crisis.
The MHS is responsible for the delivery of health care to more than 9.5 million beneficiaries eligible for the military health care benefit worldwide through 53 hospitals and more than 400 medical and dental clinics, as well as all health policy for the department. It serves as medical advisor to the White House, conducts an extensive research and development program, manages the education and training of all military medical personnel, leads a military medical university called the Uniformed Services University of the Health Sciences and conducts coordinating activities with all federal agencies including the Center for Disease and Control, Health and Human Services and the Department of Veterans Affairs. The MHS consists of Army, Navy and Air Force medical departments, a joint staff surgeon, the Defense Health Agency and the University.
During COVID-19, he is coordinating all strategic planning, operations and tactics impacting medical issues for the 9.5 million beneficiaries, managing two of the five largest DoD websites (health.mil and Tricare.mil), conducting media training, interfacing with the media, pitching stories and responding to media inquiries, leading a customer service interface program, managing a newsroom, developing outreach products for strategic partners, managing several social media platforms and serving as the senior communications advisor to the entire worldwide Military Health System.
We asked him a few questions about his work and life during COVID-19.
What does your day-to-day look like and how is that vastly different from what it looked like before the crisis?
The greatest challenge is the higher level of intensity in the daily mission and managing both the speed and accuracy of timely, critical information in an environment that changes by the minute. My day starts at 0545 hrs. (5:45 a.m.) when I receive my first media reports from the previous 24 hours. Then I work with my media team to conduct an analysis and prepare to brief senior leaders on media engagements daily at 0730 hrs. At 0800 hrs., I set the day's priorities for my team of more than 80 people. At 1015 hrs. daily, I hold a communications operations call where I receive updates from the team on worldwide communications missions. These include a situational overview of how the department is managing the crisis and the impact of the communication, the critical information that needs to be disseminated to both beneficiaries and stakeholders worldwide and updates on programs, policies and activities.
Throughout the day, there are numerous meetings, briefings, discussions, strategic advising and project guidance provided. At 1700 hrs. (5 p.m.) I have a leader’s recap, review the missions of the day and begin the plans for tomorrow. Then at 1800 hrs., I go for a long walk with my wife Lorrie (Marywood University '78), return to my computer and respond to the more than 300 emails I received throughout the day. Today’s biggest challenge (Friday, April 10) is a major media presser in the Pentagon Briefing Room.
Obviously, Communications and outreach are incredibly important at this time. How do you ensure that the entire country hears your message?
Great question and a hard question. Fortunately, my communications team has a good network and series of communications tactics developed over years of hard work, planning and outreach. The challenge is not the delivery or the dissemination of information. The real challenge is sorting through conflicting information from multiple sources to consolidate the most accurate message to be delivered to our various audiences.
Testing of the COVID-19 virus, access to care, canceling elective surgery, waiving co-pays, limiting pharmaceuticals and communicating a 500 percent increase in calls to our 24/7 nurse advice line require focused communications. Just think of the stories. The deployment of the USNS Comfort and Mercy hospital ships, the establishment of Army field hospitals, the activation of National Guard and reserve medical units, the early graduation of the Uniformed Services University of the Health Sciences medical school and graduate school of nursing, the research efforts to find a cure and the education of the military medical force are stories we try to tell worldwide. And we use multiple channels: media, our two websites, video conferences with stakeholders, internal communications, gov. delivery email blasts, video messages, daily leadership messages, graphics, are some ways. Sending products to stakeholders and encouraging them to share our communications message are also key to success.
Bottom line. Consistent, accurate, timely and credible information delivered fast over many channels contributes to success. The challenge is getting this data and validating it. And we are always looking at ways to cut through the massive news clutter. It is a real challenge. The key is finding the right, unique story that grabs the interest of the audience.
How are you coping, personally, with what is going on right now?
Keeping everyone on my team focused, encouraging personal time and family time, emphasizing exercise and movement and sometimes using comedy to put some leverage into the day. However, we experienced a tragedy recently.
On April 2, my media relations chief, Kevin Dwyer, died in his sleep. This was not COVID-19 related. At 51 years of age, the previous night, he had completed a long bike ride, spent time in his yard and called his sister saying what a great ride he had. When he did not come to work on Thursday, I sent the Alexandria, Virginia, police to his home where they found him in bed. Single with no health issues at all, we were stunned. On Friday morning at 0800 hrs., I conducted a phone call with my team to break the news to them. The hardest part is we are all separated and cannot grieve as a team.
I can handle a long day. I’m a soldier, and I have served in several crises. I am devastated at the loss of both a colleague and friend, especially during the Easter season. So, I pray a lot and do all I can to encourage my team to honor his memory through our work.
How have you relied on your training?
I totally rely on my training and experience. I was the senior spokesman as an Army Colonel on the grounds of the Pentagon for the first three weeks after the attack on 9-11 and conducted media training to the New York National Guard in New York City. As the senior Public Affairs Officer for the U.S. Army Military District of Washington, I led a wartime scenario on a battlefield in my hometown. I had a very young and inexperienced team, so my leadership was critical to success. We did two daily news conferences in front of more than 300 media daily, briefed senior leaders, dignitaries, congressional and in some case celebrities on the operation and the specifics of what happened. I have commanded six times in uniform and am very comfortable in crisis scenarios. But it is the resilience and professionalism of my teammates, not necessarily me, that gets us through a crisis. I just provide guidance. These pros execute the mission flawlessly.
Colonel Richard H. Breen, Jr. ’77: A New Mission
Colonel (R) Richard H. Breen, Jr. ’77, director of Strategic Communications for the Military Health System, guides his team through COVID-19. He talks about the challenges of his new normal, here.

As the president and CEO of Main Line Health (MLH), I have the honor and privilege of working with more than 12,000 employees and medical staff members who comprise one of the Delaware Valley’s largest health systems. In the summer of 2019, we launched a new brand campaign to capture the essence of the MLH spirit and to differentiate the experience our team strives to deliver. The foundation of the campaign was crafted after dozens of interviews with team members from across the organization to explain what drives us at MLH; to describe the values we bring forth every day to make MLH the best place to both give and receive care. This work resulted in a brand narrative that defines our promise to see, hear and connect to each of our patients as individuals, and our belief that Health Care is Human Care.
Since the arrival of COVID-19 to our region in early March, our MLH spirit has undergone the ultimate test. While the Philadelphia region, in general, had the opportunity to learn from areas severely hit with less time to plan (such as Seattle and New York City) we at MLH treated some of the earliest cases on the East Coast. In fact, Montgomery County, located directly in our service area, saw among the first COVID-19 cases in the state and by mid-March, our campuses had treated close to 20-30 percent of all the cases in Pennsylvania.
With the early signs that COVID-19 had infiltrated our communities, we implemented our incident command structure across the System and began comprehensive planning, and 24/7 coverage to ensure a coordinated response across our five hospitals. The safety of our patients, team and community always remains at the crux-of our planning and decision making. Key areas of focus for us over the past six weeks included:
- Changing processes and procedures: This included canceling elective surgeries, implementing screening checkpoints, and the suspension of volunteer services and visitor restrictions.
- Procurement of Personal Protective Equipment (PPE) for our team: Our Logistics team has literally scoured the globe to ensure our team is appropriately protected, and we secured shipments from around the world. While we believe we currently have sufficient supply, our responsibility as health care leaders is to ensure responsible and prudent use to conserve as much PPE as possible for the duration of the pandemic.
- Securing and deploying testing for the community: The MLH team was one of the first in the state to establish drive through testing for those who were ill, but did not need emergency level care. Likewise, we worked doggedly to secure rapid testing for our inpatients—this type of testing is key to appropriately managing patients and protecting our team. To date, we have tested almost 7,000 community members.
- Surge planning: Our team has created predictive modeling to anticipate when our area could experience the highest volume of cases. In order to serve as many in our community as possible, we worked extensively on a three-tiered surge model that allows us to scale our bed capabilities and use non-traditional patient areas, like large conference rooms, should it be necessary. When fully activated, we could care for 1,600 inpatients across MLH.
I am incredibly proud — and forever grateful to — our administrative team for their dedication, ingenuity, collaboration and exhaustive efforts to ensure we are operationally prepared to serve the community when they need us most. However, it’s those by the bedside — our heroes directly battling this silent enemy — whose work surpasses all expectations. These brave individuals on the front lines who provide critical care, serve as family for those patients who have none, and create a safe and clean environment are the ones who truly embody the concept that health care is human care. Despite their own fears and facing so many unknowns, these crusaders “suit up” every day, committed to saving as many possible. In the span of a day, they experience sorrow and triumph, but in response to every situation, they respond with strength and grace.
Take for instance Lindsey, a nurse caring for a COVID-19 hospice patient. As the virus took this patient’s life, several family members visited throughout the day, but all had just gone home for the night. Due to the set-up on the unit, Lindsey was able to see directly into the patient’s room from the nurses station. Within a short span of time, she noticed an acute change in her patient's status. She gowned as quickly as possible to enter the room and spend the last 3-4 minutes of her patient’s life by their side. When the physician called the family to share the news of their loved one’s death, she was also able to offer the solace that Lindsey was present at the bedside… their parent did not die alone.
While we mourn those taken by COVID-19, we also celebrate our survivors. Such as when one of our Hospital teams arranged a joyous farewell for a patient who spent more than 20 days in the Intensive Care Unit, on a ventilator. Just as the lives that are lost leave scars on our team, this patient, too, leaves an indelible imprint on our front-line heroes. It is these moments that offer a revitalizing reminder of why we are in this work, after all. While there can be profound sadness in health care, there is also unforgettable joy.
These moments demonstrate compassion and empathy that represent not only the MLH spirit but the human spirit. This pandemic has taken lives, upended the financial infrastructure of our nation, and altered daily existence as we have known it for so long. But it’s also given something to us … these human moments. Moments that demonstrate the goodness of humanity. Moments that allow our faith to shine. Moments that give us strength and hope for a future that is far brighter than we could have possibly imagined.
Something Found in COVID-19: Human Moments
Jack Lynch '83 writes about his experience during the COVID-19 crisis as president and CEO of Main Line Health.

When World Languages and Cultures Professor Emerita Linda Ledford-Miller, Ph.D., began sewing at the age of 9, she never imagined that one day she would be home-bound, making masks to be used by healthcare workers and others responding to a worldwide pandemic.
Yet, that is what the recipient of four Fulbright fellowships finds herself doing almost on a daily basis.
“To date I have finished 150 masks, and I have another 33 ready for the pressing and pleating and stitching that I'll probably finish today,” said Dr. Ledford-Miller. She first began making masks on Mar. 21 in response to a Facebook post by a complete stranger calling for cloth masks. She found a pattern for masks on the website of Deaconess Hospital in Evansville, Indiana, and went to work. Initially, she made about 6 masks per day, but then refined her approach to more of a “production model” she said – prepping materials one day, then pinning them for sewing, etc. on another. “So somedays I make none, then have 25 finished the next day,” said Dr. Ledford-Miller.
Dr. Ledford-Miller has sent her masks to a number of organizations and places, including Friends of the Poor, the Mulberry Street Fire Station and Masked Bandits, which is a combined effort of the Luzerne and Lackawanna Medical Societies to collect donated cloth masks. She has also sent masks to friends and family members and even to the daughter of a faculty member who is serving as nurse at Vanderbilt University Medical Center in Tennessee.
Dr. Ledford-Miller recalls her first sewing project, at the age of 9, was “a ‘broom skirt’ – a piece of fabric with a hem and elastic waist. My next project was a suit – a matching skirt and blouse with scotties on it. My mother said it was too advanced for me, but I was stubborn and made it anyway.”
Today, health professionals and others affected by the Covid-19 pandemic are benefiting from her hobby – and her tenacity.
Professor Puts Hobby to Good Use
Professor turns to hobby to answer call for cloth masks needed for Covid-19 pandemic responders.
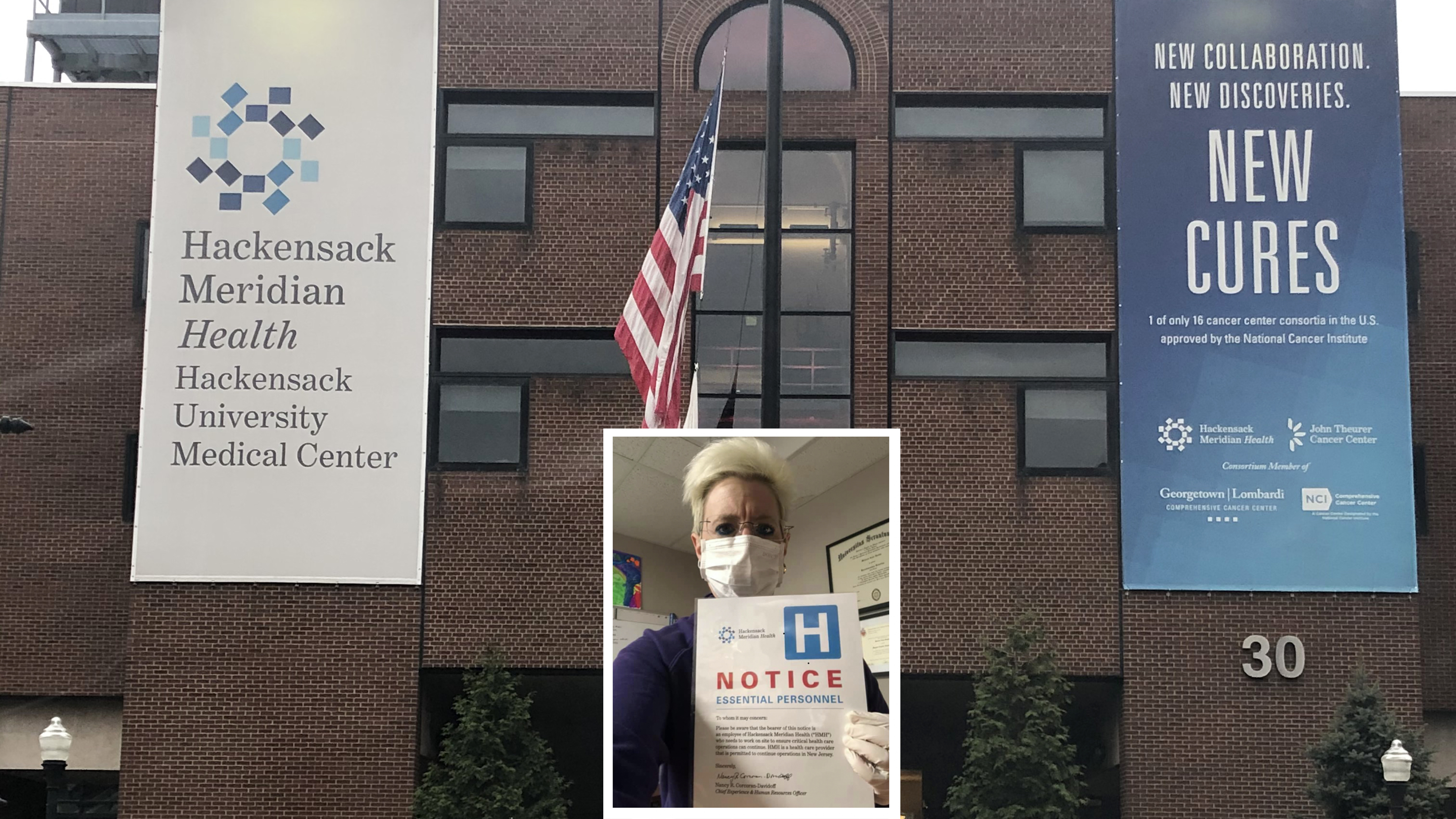
When people think of front-lines health care workers, they rightfully imagine those in direct care.
But legions behind the scenes fuel the critical work of the front lines, and University accounting graduate Melissa Schnipp ’96, of Bogota, New Jersey, is among them. So are her 10-year-old son, Antonello, and husband, Dan.
Melissa is site finance controller at Hackensack Meridian Health’s Palisades Medical Center, a community hospital increasing its ICU beds and converting floors to serve a community hard-hit by COVID-19. Her role in this pandemic, she explained, is “keeping the cash flow moving, monitoring the materials supply chain, pushing all the paperwork through and making sure emergency purchasing gets accomplished.”
At Hackensack Meridian, workers in many roles have been redeployed as the virus progressed, and Melissa has been no exception. Originally working from home when the crisis became full-blown, she had been, at points, called back to the physical site to play various roles. It was during her time at home, though, when some bonus family bonding led to a special mission for the Schnipps, initiated by Antonello.
While Melissa was working at home, she said, her family heard more than usual of one another’s work or school conversations, giving her a new understanding of her husband’s and son’s days and them of hers.
“They got to hear some of the safety calls and the things we talk about every day,” she said. Antonello, understandably, had been worried about his mother, especially when she was going into the medical center.
“I just reassured him that I was going in to help, and that this is what we need to do for society as a whole,” she said, noting that value was formed early on while a student at Scranton.
“He asked why there wasn’t a cure, and I explained we need research,” she recalled.
Antonello had an idea. Having already dabbled in fundraising efforts, raising money for childhood cancer and for the American Heart Association, he asked Melissa if he could raise dollars to help find a COVID-19 vaccine.
He explained his mission as simply as any 10-year-old would: “I wanted to get research so people wouldn’t get sick and nobody would die.”
The Schnipps used the Hackensack University Medical Center Foundation’s platform to set up a personal page, The “Big A COVID-19 Combat Fund.”
“Because he is 10 we set the goal at $1,000 and told him we’d match whatever he was able to raise,” Melissa said. “We sent emails out and a few Facebook posts using the URL link for his team site."
The page reached its goal in a week, has now hit $1,150 and is still active. The money will go to Hackensack Meridian’s Center for Discovery and Innovation, which is researching and working on a vaccine.
Scranton, Melissa said, laid the groundwork for this.
“Dean Michael Mensah taught me well,” she said. “He always stressed we were going to face things in life that were not ‘textbook.’ When we got into the world, we would need to be prepared for anything.”
“That lesson really resonates with me now,” Melissa said, as does the way the University stressed service. “My compassion and passion for service – and my trying to instill the same in my son – definitely came from Scranton.”
A Family Fundraising Effort from Behind the Frontlines
The work of Melissa Schnipp ’96, site finance controller at Hackensack Meridian Health’s Palisades Medical Center, inspires her 10-year-old son to get involved in the fight against COVID-19.
The University of Scranton's Nursing Department thanks all the alumni RoyalRNs out in the world doing work to combat COVID-19 in this video tribute.
Nursing Department Thanks Alumni RoyalRNs
The University of Scranton's Nursing Department thanks all the alumni RoyalRNs out in the world doing work to combat COVID-19 in this video tribute.